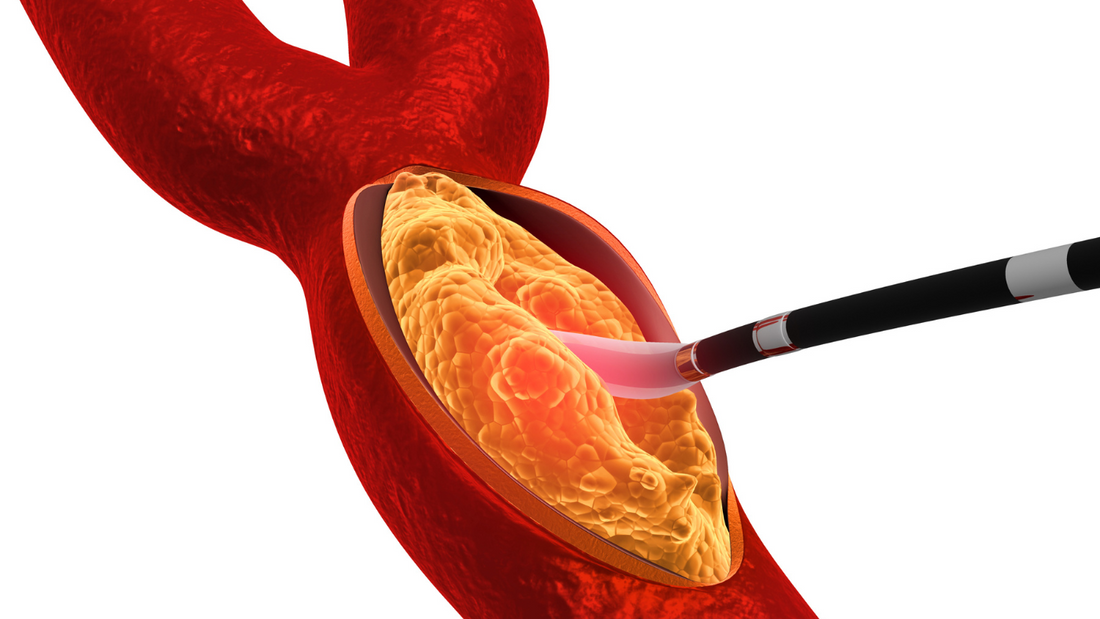
Arteries become blocked due to a build-up of plaque, which is a sticky substance made up of fat. This build-up is called atherosclerosis, and it can cause arteries to narrow or harden. When arteries become blocked, blood flow to the body is reduced, increasing the risk of serious cardiovascular events like heart attacks and strokes.
Some risk factors for atherosclerosis include:
-
High Blood Pressure (Hypertension)
-
Damage to Artery Walls: High blood pressure puts extra force on the walls of arteries, causing damage to the endothelium (the inner lining of blood vessels). This damage makes it easier for substances to build up and form plaque.
-
Chronic Strain on the Heart: Persistent high blood pressure can also make the heart work harder, increasing the risk of the heart muscle thickening and narrowing of the arteries.
-
-
Smoking and Tobacco Use
-
Direct Damage to Arteries: Chemicals in tobacco smoke can damage the endothelium, making it more susceptible to plaque formation.
-
Increased Blood Clotting: Smoking increases the tendency for blood to clot, which can accelerate the process of atherosclerosis.
-
-
Obesity and Physical Inactivity
-
Excess Weight: Obesity is associated with several risk factors, including insulin resistance, both which contribute to the development of atherosclerosis.
-
Sedentary Lifestyle: Lack of physical activity can worsen these risk factors, as regular exercise helps to maintain a healthy heart.
-
-
Family History of Heart Disease
-
Genetic Predisposition: A family history of heart disease or early-onset atherosclerosis increases the likelihood of developing this condition, as certain genetic factors can influence blood pressure and the risk of inflammation in the arteries.
-
The major controllable risk factors include smoking, poor diet, and physical inactivity. Controlling these factors can significantly reduce the risk of developing atherosclerosis. Non-modifiable risk factors like age, genetic predisposition, and family history should be monitored with regular check-ups and a heart-healthy lifestyle.
By addressing the modifiable risk factors and working with healthcare providers, individuals can reduce the likelihood of atherosclerosis and maintain better cardiovascular health.
Can Atherosclerosis Be Cured?
We have testimonials from users of the Heartstrong protocol who have been able to reverse the build-up of arterial plaque, as shown by improvements in their CAC (Coronary Artery Calcium) scores. While atherosclerosis cannot be completely cured, it can be managed, stabilized, and in some cases, significant regression has been demonstrated. Our focus is on preventing progression, reducing symptoms, and lowering the risk of complications such as heart attacks and strokes. Here’s a closer look at what can be done to manage atherosclerosis:
Lifestyle Modifications:
-
Supplement Support: Taking supplements like serrapeptase and nattokinase, along with vitamins D3 and K2, can support optimal calcium reallocation, potentially aiding in the prevention of arterial plaque buildup. These supplements work together to support healthy blood flow and cardiovascular health, offering a natural approach to managing atherosclerosis.
-
Healthy Diet: Adopting a diet that is rich in fruits, vegetables, whole grains, and healthy fats (like those from nuts, olive oil, and fatty fish). The Mediterranean diet is often recommended for heart health.
-
Regular Exercise: Physical activity helps improve blood flow and lower blood pressure. Even moderate exercise, like walking, swimming, or cycling, can have significant benefits.
-
Weight Management: Losing excess weight can reduce many risk factors associated with atherosclerosis, including high blood pressure and insulin resistance.
-
Quitting Smoking: Smoking damages the blood vessels and accelerates the process of plaque buildup. Quitting smoking is one of the most effective steps to slow the progression of atherosclerosis and reduce the risk of cardiovascular events.
Interventional Procedures and Surgery
-
Angioplasty and Stenting: In cases where atherosclerosis has significantly blocked an artery, a minimally invasive procedure called angioplasty may be performed. A small balloon is used to widen the artery, and a stent (a small mesh tube) is placed to keep it open.
-
Coronary Artery Bypass Grafting (CABG): For more severe blockages, especially in the coronary arteries, bypass surgery may be necessary. In this procedure, a healthy blood vessel is taken from another part of the body and used to create a new pathway around the blocked artery.
-
Carotid Endarterectomy: For blockages in the carotid arteries (the main arteries to the brain), this surgical procedure removes plaque directly from the artery to restore blood flow.
Managing Other Risk Factors
-
Diabetes Management: Keeping blood sugar levels under control is crucial for people with diabetes, as high blood sugar can accelerate plaque formation. Managing diabetes through diet, exercise, and medications can help reduce the impact of atherosclerosis.
-
Managing Stress: Chronic stress is linked to higher levels of inflammation and blood pressure, which can worsen atherosclerosis. Stress management techniques like meditation, yoga, and mindfulness can contribute to overall heart health.
What is vitamin k2 and how it can help me.
Vitamin K2 is gaining attention for its potential benefits in cardiovascular health, particularly regarding its role in preventing arterial calcification and supporting overall heart and blood vessel function. It may help your body in it's ability to reduce the progression of atherosclerosis and calcium buildup, which are key factors in arterial blockages. Here’s how Vitamin K2 may assist in maintaining healthier arteries:
Role Of The Vitamin K2 in Preventing Vascular Calcification
-
Directing Calcium to the Bones: Vitamin K2 plays a crucial role in activating certain proteins that help direct calcium into the bones and teeth, where it’s needed, rather than allowing it to accumulate in soft tissues like arteries. The protein osteocalcin, for example, is activated by Vitamin K2 to bind calcium in bones.
Reducing the Progression of Atherosclerosis
Slowing Plaque Formation: Atherosclerosis involves both the buildup of cholesterol-rich plaque and the calcification of these plaques. Vitamin K2 supports your body’s natural ability to slow the progression of atherosclerosis by helping to reduce the calcification process, keeping plaques more stable and less prone to hardening and narrowing the arteries.
Maintaining Arterial Elasticity: By aiding in the reduction of calcium buildup in the arterial walls, Vitamin K2 helps your body naturally maintain blood vessel flexibility and elasticity. This elasticity supports free-flowing blood circulation, reducing the risk of restricted blood flow and cardiovascular events like heart attacks and strokes.
Vitamin K2 Working Together with Vitamin D3
Synergy with Vitamin D3: Vitamin K2 and Vitamin D3 work in harmony to support your body’s natural heart health processes. While Vitamin D3 aids in calcium absorption, Vitamin K2 helps ensure that this calcium is directed to the bones and kept out of the arteries, helping to maintain bone strength without contributing to vascular calcification.
Balancing Calcium Levels: Without sufficient Vitamin K2, an increase in Vitamin D3 intake may lead to calcium deposits in arteries rather than its intended use in bones. By combining Vitamin K2 with Vitamin D3, your body can naturally optimize calcium metabolism and reduce the risk of arterial calcification, promoting better cardiovascular health.
How to Get Enough Vitamin K2
Dietary Sources: Foods rich in Vitamin K2 include natto, fermented cheeses, eggs, and certain meats like liver. Natto is one of the best sources, particularly of MK-7.
Supplements: Given that many diets are low in Vitamin K2, supplementation is a common option, especially for those who are looking to improve their cardiovascular health.
Important Considerations
Vitamin K2 can be a valuable ally in maintaining artery health by preventing calcium from depositing in the arterial walls, thus helping to reduce the risk of hardening and narrowing of the arteries. By keeping calcium where it belongs—in the bones—it helps support flexible, healthy blood vessels, which is critical for preventing the progression of atherosclerosis. While it won't directly remove existing blockages, it can play a role in slowing down further calcification and supporting overall cardiovascular health.
At Heartstrong Nutraceuticals, our protocol includes Vitamin K2 and D3, carefully selected for their synergistic benefits in supporting cardiovascular health. These supplements are an essential part of our approach, designed to assist the body’s natural ability to manage arterial health and reduce atherosclerosis progression.